Simon J. Wheeler, BVSc, PhD, DECVN, Dipl Mgmt, FRCVS (Veterinary Neurology)
Cervical spinal surgery has made significant progress in the last 20 years, when operations were largely restricted to cervical fenestration for disc herniations. At the time, decompression of the spinal cord vial ventral 'slot' was starting to be considered and this has become the 'gold standard' surgical therapy for this disease. Advances have also been made in the treatment of atlanto-axial subluxation and the surgical management of cervical spondylomyelopathy (CSM--'The Wobbler Syndrome').
More information can be found in Small Animal Spinal Disorders, 2nd edition, by NJH Sharp & SJ Wheeler, Elsevier, London. Available from www.veterinary-neurology.com.
Cervical Disc Disease
Cervical disc disease is a frequent disorder of dogs. Small dogs are affected commonly, particularly those with chondrodystrophoid characteristics although the condition can occur in any breed. Dachshunds, Beagles, Poodles, Spaniels, Shih Tzus, Pekinese and Chihuahuas are affected most often. Large breed dogs also suffer from cervical disc disease, usually as part of the syndrome of caudal cervical spondylomyelopath. Most small dogs suffer signs after two years of age, with a mean of six years.
The predominant clinical sign is severe neck pain, which may be acute or chronic. This is one of very few conditions that cause dogs to scream spontaneously. Often the pain is unremitting and not responsive to medication although dogs with more marked neurological deficits show less pain. Affected dogs may be reluctant to eat unless the food is raised off the floor.
Neurological deficits may be restricted to one thoracic limb or the dog may show hemiparesis, tetraparesis or even tetraplegia with hypoventilation. Neurological deficits are more common with lesions at C4/5 to C6/7 inclusive, while neck pain without deficits is more common with lesions at C2/3 and C3/4.
Diagnosis is based on the clinical signs described above. On survey radiographs, narrowing of the intervertebral space or dorsal displacement of mineralised disc material provides supportive evidence. Myelography or advanced imaging are necessary for definitive diagnosis. Survey radiographic features of disc disease are common incidental findings in older dogs.
Analysis of CSF is useful to eliminate inflammatory disease. Results of CSF analysis may be abnormal in disc disease, but elevations of protein and cells are usually mild.
Myelography or advanced imaging are necessary to confirm the diagnosis (Figure 1).
Click on the image to see a larger view.
| Figure 1. | 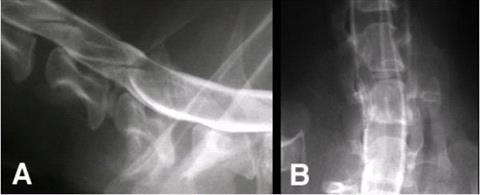
A: Lateral myelogram from a 10-year-old Shih Tzu that presented with neck pain and no neurological deficits. There is a narrow intervertebral space at C5/6 with splitting of the ventral contrast column at this level (see 4.23-25). B: Dorsoventral myelogram. |
|
| |
Computed tomography is also valuable. Depending on the scanner, CT is usually much faster to perform than myelography and may be more accurate for surgical planning. When available, CT is the imaging modality of choice for chondrodystrophoid dogs with suspected cervical disc disease. The cross sectional image helps the surgeon to plan the ventral slot and is also very useful to identify lateralised or foraminal lesions (Figure 2).
Click on the image to see a larger view.
| Figure 2. | 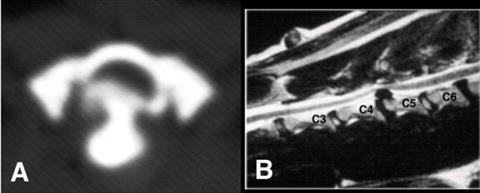
A: CT scan through C5/6 made after myelography of patient shown above The connection between the disc extrusion and the rest of the nucleus pulposus is seen clearly. B: T2-weighted, sagittal MRI to show a disc extrusion at C4/5. The adjacent discs are of relatively normal signal intensity but the C2/3 and especially the C6/7 discs are degenerate with low signal intensity. |
|
| |
Treatment may be non-surgical or surgical. Non-surgical treatment entails cage rest and use of anti-inflammatory medications. It can be tried in any patient unless marked neurological deficits are present. Progression of signs or lack of response in one or two weeks indicate treatment failure. A dog that is responding well to non-surgical treatment should be kept rested for at least two weeks after clinical signs have resolved. Recurrence of clinical signs after non-surgical treatment has been reported in over 30 per cent of patients.
Indications for surgical treatment include:
 Failure of non-surgical treatment
Failure of non-surgical treatment
 Unremitting pain
Unremitting pain
 Severe or progressive neurological deficits
Severe or progressive neurological deficits
Ventral decompression is the preferred procedure. It may need to be combined with fixation for caudal disc extrusions. Dorsal or dorsolateral decompression may be required in disc extrusions that cannot be reached via ventral slot or if there is doubt about the diagnosis.
Although the value and desirability of fenestration has been questioned, it should prevent further herniation of disc material into the vertebral canal and so reduce the recurrence rate. It also appears effective for dogs with discogenic pain. It is usual to fenestrate the discs from C2/3 to C5/6 inclusive; C6/7 is fenestrated if there is evidence of disease.
General indications for decompression include:
 Presence of neurological deficits
Presence of neurological deficits
 Spinal cord compression on neuroimaging
Spinal cord compression on neuroimaging
 Failure of fenestration
Failure of fenestration
Removal of disc material by ventral slot decompression provides the most rapid resolution of clinical signs and it is therefore the treatment of choice. Accurate identification of the disc involved is an obvious prerequisite. The width of the slot should be about one-third the width of the vertebral body and certainly no more than 50 %.
Postoperative instability or subluxation are important potential complications that can be prevented by fixation of the interspace at the time of ventral decompression. Fixation is not necessary for cranial disc lesions (C2/3 and C3/4) but should be performed for caudal lesions (C4/5 to C6/7) when the slot width is 50 % or greater.
Atlanto-axial subluxation
Clinical signs in congenital atlantoaxial subluxation are usually seen in immature patients although signs can develop later in life. The disorder is encountered most often in small breeds of dog, particularly Yorkshire terriers, Chihuahuas and Miniature poodles. Rare cases occur in large breed dogs and cats. Neck pain is seen in most dogs. Neurological signs reflect cervical spinal cord compression. In mild cases only conscious proprioceptive deficits are seen. Tetraparesis indicates more significant spinal cord compression. Survey radiographs provide the diagnosis in most cases (Figure 3).
Click on the image to see a larger view.
| Figure 3. | 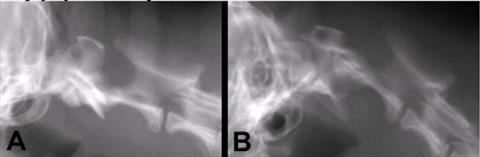
Survey radiographs from a one-year-old Toy poodle showing a marked increase in the gap between the dorsal arch of C1 and the spinous process of C2. |
|
| |
Surgical treatment is indicated in most patients with congenital lesions. Even dogs with profound neurological deficits are likely to benefit from stabilisation. The two main options are either ventral fusion or dorsal stabilisation. Ventral fusion is the treatment of choice.
Fusion of the atlantoaxial joints can be performed using either transarticular fixation or using multiple implants and bone cement. Good results can be obtained using transarticular fixation; threaded pins or screws give superior results to smooth pins (Figure 4).
Click on the image to see a larger view.
| Figure 4. | 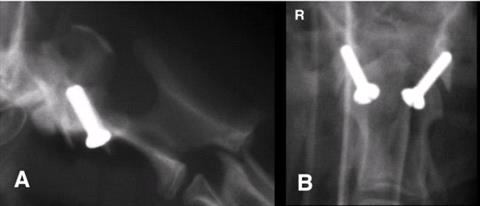
Reduction after transarticular screw fixation is good in this case. |
|
| |
Cervical Spondylomyelopathy
Cervical spondylomyelopathy (CSM) ("Wobbler syndrome") is predominantly a syndrome of large and giant breed dogs, particularly Doberman pinschers and Great Danes. The cause of this disorder is multifactorial. Important contributing factors are:
 Vertebral canal malformation, stenosis, or both
Vertebral canal malformation, stenosis, or both
 Vertebral instability
Vertebral instability
 Ligament hypertrophy
Ligament hypertrophy
 Joint capsule proliferation or cyst formation
Joint capsule proliferation or cyst formation
 Osteophyte production
Osteophyte production
 Disc herniation
Disc herniation
Clinical signs usually develop due to acquired soft tissue or osseous lesions; these are probably as a consequence of low-grade instability. An early onset of clinical signs is most common in giant breed dogs. Most other breeds show signs from middle age onwards. Compression is seen mainly at C5/6 & C6/7 in the Doberman but lesions in other breeds may affect more cranial disc spaces.
The most common presentation is a gait disturbance, which is most severe in the pelvic limbs and ranges from mild ataxia to marked paresis and dysmetria. Cervical hyperaesthesia, guarding of the neck, pain on manipulation of the prominent transverse process of C6 or a low carriage of the head may also be seen.
Survey radiographs are useful to rule out potential differential diagnoses but are not definitive for CSM. Myelography is the standard means of confirming a diagnosis of CSM and has the advantage that the lesion can be observed readily in different positions of the spine. Ideally all conventional myelograms for CSM should be followed by a CT scan. The CT provides excellent bone imaging and with contrast it also gives a good transverse image of the spinal cord. This information can improve surgical planning and may provide prognostic information by detecting spinal cord atrophy.
This is the technique of choice for imaging humans with degenerative diseases of the cervical spine. It is non-invasive and also provides superior soft tissue resolution to CT-myelography.
The decision on the best way to treat each patient is based on the presenting history, neurological status, results of imaging, and on the owner's expectations and their ability to undertake any necessary aftercare. Most dogs that show neurological deficits are surgical candidates, but consideration should also be given to non-surgical treatment, which is warranted in two situations. The first is when a dog develops neurological deficits following minor trauma. The second is when a dog develops CSM before it is skeletally mature and so may benefit from correction of nutritional imbalances together with severe caloric reduction. For most other dogs, however, surgery is the treatment of choice as the majority probably show progressive deterioration.
For most other dogs with CSM surgery is elective and so a two to four week trial period of severe exercise reduction and use of a chest harness is often justified. Anti-inflammatory doses of prednisolone may also be used, but for short periods only and preferably on an alternate day basis.
A large number of different surgical techniques have been proposed for CSM, with many of the authors claiming between 70 and90 per cent success rates. The most logical way to obtain the best overall results is to consider three basic types of surgery and to perform these for certain, relatively well defined indications. The three types of surgery are:
 Ventral decompression
Ventral decompression
 Vertebral stabilisation and distraction
Vertebral stabilisation and distraction
 Dorsal decompression
Dorsal decompression
The main factor governing the choice of surgical procedure is the appearance of the spinal cord on imaging, particularly the traction and flexion views after myelography. Some lesions show a combination of different types of compression and then a judgment must be made as to which is the major component. In general:
 Dogs with single, ventral lesions that do not respond to traction should undergo a ventral slot.
Dogs with single, ventral lesions that do not respond to traction should undergo a ventral slot.
 Single and multiple lesions that respond well to traction should undergo cement plug distraction stabilisation. Ventral slot can be as good for single lesions if done very well.
Single and multiple lesions that respond well to traction should undergo cement plug distraction stabilisation. Ventral slot can be as good for single lesions if done very well.
 Single and multiple lesions that are positional should undergo cement plug distraction-stabilisation. Some surgeons may prefer a dorsal decompression, particularly for dorsal positional lesions.
Single and multiple lesions that are positional should undergo cement plug distraction-stabilisation. Some surgeons may prefer a dorsal decompression, particularly for dorsal positional lesions.
 In all dogs that show compression at only one interspace, consideration should also be given to a strategy that will prevent compression developing at adjacent high-risk spaces in the future.
In all dogs that show compression at only one interspace, consideration should also be given to a strategy that will prevent compression developing at adjacent high-risk spaces in the future.
The seriousness of this condition is best illustrated by the fact that a quarter of dogs with CSM in one series were euthanised within six weeks of surgery for neurological problems. Overall long term mortality rates for CSM vary from 19%-43%. Dogs with more than one lesion generally have a worse prognosis than dogs with single lesions, and dogs with chronic tetraparesis have a very guarded prognosis. Most severely tetraparetic dogs that are going to recover will do so within six weeks. In some dogs surgery will only halt the progression of disease, presumably because there is often significant loss of neural tissue at the site of the lesion. It is therefore likely that the outcome will be better if surgery is done earlier in the disease process.