What is a Mast Cell?
A normal mast cell is part of our immunologic defense systems against invading organisms. Mast cells are meant to participate in the war against parasites (as opposed to the war against bacterial or viral invaders). They are bound within tissues that interface with the external world such as the skin, respiratory or intestinal tract. They do not circulate through the body.
Fine Needle Aspirate From Dog's Scrotal Tumor Showing Mast Cells - Microphotograph
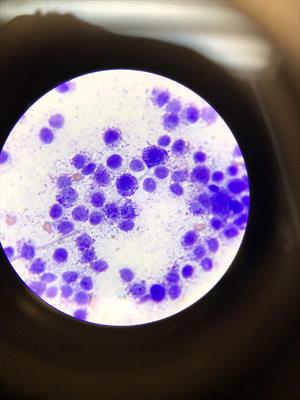
Cytology (microscope) showing mast cells taken from an inflamed scrotum of a dog with a rapidly progressing lesion. Courtesy Dr. Avery Tomlinson
The mast cell possesses granules of especially inflammatory biochemicals meant for use against invading parasites. Think of these as small bombs that can be released. The mast cell has binding sites on its surface for a type of antibody called IgE. IgE is produced in response to exposure to antigens typical of parasites (i.e., worm skin proteins, or similarly shaped proteins). IgE antibodies, which are shaped like tiny Ys, find their way to a tissue mast cell and perch there. With enough exposure to the antigen in question, the mast cell may be covered with Y-shaped IgE antibodies like the fluff of a dandelion. The mast cell is said, at this point, to be sensitized.
As said, the IgE antibodies are Y-shaped. Their foot is planted in the mast cell while their arms lift up hoping to capture the antigen for which they were individually designed. When the antigen comes by and is grasped by the IgE antibodies, this should indicate that a parasite is near and the mast cell, like a land mine, degranulates releasing its toxic biochemical weapons. These chemicals are harmful to the parasite plus they serve as signals to other immune cells that a battle is in progress, and for them to come and join in.
The problem is that we live in a clean world without a lot of parasites. What unfortunately tends to happen is that the IgE/mast cell system is stimulated with other antigens that are of similar shape or size as parasitic antigens. These next best antigens are usually pollen proteins and the result is an allergy. Instead of killing an invading parasite, the mast cell biochemicals produce local redness, itch, swelling, and other symptoms we associate with allergic reactions.
And the Mast Cell Tumor?
As if the mast cell isn't enough of a troublemaker in this regard, it can form a tumor made of many mast cells. When this happens, the tumor cells are unstable. This means they release their toxic granules with simple contact or even at random, creating allergic symptoms that do not correlate with exposure to any particular antigen. Simply handling the tumor can cause it to degranulate, leading to redness, itching, and/or swelling. Growths that get suddenly larger and then smaller over a 24-hour period are likely to be mast cell tumors and this phenomenon is referred to as Darier's sign.
Furthermore, mast cell tumors are notoriously invasive and difficult to treat. Part of the problem is that what appears to be the visible margin of the tumor is rarely the actual margin. (Picture an octopus where the body is part of the tumor you see, but there are invisible tentacles extending out in many directions.) Because it is not possible to see the true tumor margins with the naked eye, excision must be broad and deep and the tumor may not be located on a part of the body where this is possible.
Canine
Mast cell tumors are the most common skin tumor in dogs, with between seven and 21 percent of all canine skin tumors being mast cell tumors. Mast cell tumors do not have to involve the skin and can develop internally but most of the time there is skin involvement. While any dog can develop a mast cell tumor, several breeds have an especially high rate of mast cell tumor development (four to eight times the rate of the general canine population). These breeds are the boxer, the Rhodesian ridgeback, the pug, the Boston terrier, the pit bull terrier, and the Weimaraner. The Shar-pei tends to develop its mast cell tumors at an earlier age and they tend to be especially malignant.
Diagnosis can often be made with a needle aspirate, which collects some cells of the tumor with a needle, and the cells are examined under the microscope. The granules have distinct staining characteristics leading to their recognition. An actual tissue biopsy, however, is needed to grade the tumor, and grading of the tumor is crucial to determining prognosis.
Mast Cell Tumor, Lip, Dog (Photograph)

Dog with mast cell tumor on lip. Courtesy of Dr. Scott Vaughan
Grading the Mast Cell Tumor: The Patnaik System and the Kiupel System
The pathologist will most likely use both of these systems to grade the mast cell tumor. The grade is a reflection of the malignant characteristics of the cells under the microscope (which of course generally correlates to the behavior of the tumor). In the Patnaik system, mast cell tumors are graded either I, II, or III with Grade I being benign, Grade III being malignant, and Grade II having some ability to go either way. In the Kiupel system, which was designed to clear up some of the ambiguity of the Grade II tumors, the mast cell tumor is simply classified as low-grade or high grade with high-grade tumors far more likely to behave malignantly.
Grade I Tumors
This is the best type of mast cell tumor to have. While it may tend to be larger and more locally invasive than may be visually apparent, it tends not to spread beyond its place in the skin. Surgery should be curative and no chemotherapy or other treatment is generally needed. That said, the tumor is still octopus-shaped with tentacles that extend away from the visible growth. This means that if the entire tumor has not been removed, it has the potential to grow back in its original location.
The biopsy report will include margins, which refer to the amount of tumor-free tissue surrounding the tumor tissue. If the original biopsy sample shows that the tumor has only narrowly been removed (narrow margins) or that the tumor extends to the margins of the sample (dirty margins), you have real potential for the tumor to regrow. If you wish to permanently remove the tumor, a second surgery will be needed to take away more tissue. The grade I tumor is unlikely to involve anything other than local irritation but, again, if the margins are not clean, consider a deeper resection. About half of all mast cell tumors are Grade 1 tumors and can be cured with surgery alone.
Grade II Tumors
This type of tumor is somewhat unpredictable in its behavior, which makes it difficult to determine how aggressive one should be in staging, treating, etc. Additional staining of the tumor with silver particles (AgNor staining), for c-kit granule patterns, and other structures is sometimes used. Many reference laboratories will offer staining packages to elucidate all the possible factors that have been investigated as possible indicators of malignant behavior. These staining tests have been fraught with controversy, which brings us to another factor that helps predict tumor behavior: the mitotic index. This index examines the tumor for cells in the active process of division in a given moment to get an idea of how rapidly the tumor is growing. The higher the index, the more malignant the tumor is expected to be. (Dogs with a mitotic index of 5 or less with a grade II tumor had a median survival time of 70 months vs. dogs with a mitotic index of greater than 5 who had a median survival time of 5 months). The mitotic index turns out to be an important predictor of behavior, which brings us to the Kiupel Grading System.
Grade III Tumors
This is the worst type of mast cell tumor to have. Grade III tumors account for approximately 25 percent of all mast cell tumors and they behave invasively and aggressively. They will readily spread to the spleen, liver, and bone marrow and can have extensive skin involvement. Surgery alone is unlikely to control a Grade III tumor and adjunctive treatment of some type is likely going to be necessary. What that should entail will depend on several other factors such as the location of the tumor, results of staging etc.
Grading with the Kiupel System
The Patnaik system has been in use for a long time but its grading system is somewhat subjective and every pathologist may not classify a given mast cell tumor into the same grade. The Kiupel system attempts to make the process more objective by using the mitotic index. To determine the tumor's mitotic index, 10 high-power microscopic views (fields) of the tumor are examined for cells in the process of division. The mitotic index refers to the number of actively dividing cells per 10 high-power fields. Based on variations in cell nucleus size, the frequency of finding cells with more than 3 nuclei, and a mitotic index of higher or lower than 7, the tumor is either high grade or low grade.
High Grade Mast Cell Tumors
These tumors share a universally bad prognosis with survival times of less than four months. They behave aggressively and require more aggressive therapy.
Low-Grade Mast Cell Tumors
These tumors overall showed a median survival time of greater than two years but there were some tumors that behaved aggressively despite their low grade. Additional factors add to what makes a better or worse prognosis when it comes to low-grade tumors. These factors are reviewed below.
What Comes After Diagnosis?
After the mast cell tumor has been confirmed and graded, the next steps are geared towards identifying factors that will determine prognosis and/or might limit the therapy options. Relevant factors to prognosis include: the grade and mitotic index of the tumor (which we have already discussed), the tumor staging (how far it has spread so far), tumor margins (how much tumor is leftover after surgical removal), the location of the tumor on the body, and concurrent health issues.
Basic Blood Work
Most likely a basic blood panel has been obtained and evaluated by this point but certainly, if it hasn't this would be the time. This testing will help show any factors that limit kidney or liver function and thus determine what drugs of chemotherapy can or cannot be used. It also will show if there are circulating mast cells in the blood (a very bad sign) or if anemia (low red blood cell count) is present which might be related to the tumor.
Staging the Mast Cell Tumor
In order for a rational therapeutic plan to be devised, the extent of tumor spread (or stage of the tumor) must be determined. The World Health Organization has determined a clinical staging system based on the body areas affected by the tumor. Between the stage and the grade, a plan can be devised. The tumor is staged 0 through IV as described below:
- Stage 0: one tumor but incompletely excised from the skin (i.e. dirty margins).
- Stage I: one tumor confined to the skin with no regional lymph node involvement.
- Stage II: one tumor confined to the skin but with regional lymph node involvement present.
- Stage III: many tumors or large deeply infiltrating tumors, with or without lymph node involvement.
- Stage IV: any tumor with distant spread evident. This stage is further divided into substage a (no clinical signs of illness) and substage b (with clinical signs of illness). In order to determine the tumor stage some probing of other lymphoid organs must be performed.
In order to stage the tumor, chest radiographs are typically obtained to evaluate lymph nodes in the chest. Any enlarged lymph nodes are aspirated for cell samples as are any lymph nodes local to the original tumor (regardless of enlargement). Ultrasound of the abdomen is performed to evaluate the spleen and liver. The spleen and liver are frequently aspirated as well to look for mast cells. The bone marrow may be sampled to see if there is mast cell infiltration there.
Therapy
Mast cell tumors in the following areas tend to behave more malignantly than their grade would suggest: nail bed, genital areas, the area around the anus, muzzle, ear flap, and mouth.
Therapy for mast cell tumors consists of surgery, radiation therapy, and chemotherapy (as is the case for almost all types of cancer). What combination of the above is chosen depends on the extent of spread and malignant characteristics of the tumor.
Surgery
If the tumor can be cured with one or even two surgeries, this is ideal. Mast cell tumors are highly invasive, and very deep and extensive margins - at least 2 cm in all directions - are needed. This can be a problem for tumors located on the neck or in the mouth. Further, the inflammation associated with manipulating the tumor can lead to extra swelling, bleeding, and even a drop in blood pressure. In one study, a 10% incidence of wound healing failure (dehiscence) was observed with mast cell tumors.
The biopsy sample will not only yield the grade of the tumor but will include a measurement of the tissue margin (the width of normal tissue that has been excised around the tumor). The width of the margins will go far in determining if further treatment is needed. If the margins are narrow or margins indicate there is still a tumor left behind then a second surgery or even a course of radiation therapy may be desirable. Clean margins are generally defined as a 20 mm margin around the tumor in all directions. If the margin is clean, theoretically the tumor should be completely removed but it is still a good idea to keep an eye on the area over the years.
Radiation Therapy
While radiation therapy tends to be expensive and requires a facility that may not be conveniently located, radiation has the potential to permanently cure a grade I or II mast cell tumor. Radiation is most appropriate for localized disease. If the tumor stage suggests a more distant spread is likely, radiation becomes less helpful and medications (chemotherapy) that can be delivered to the tumor through the patient's blood vessels are needed.
In January 2004, Hahn, King, and Carreras published a study where radiation therapy was used to treat incompletely removed Grade III mast cell tumors. They studied 31 dogs with Grade III mast cell tumors that did not show evidence of distant spread beyond the external area where the tumor was first detected. They treated these dogs with radiation sessions given three days a week for a total of 18 sessions. Approximately 65% of dogs achieved remission and 71% were alive one year after treatment. The median remission time was approximately 28 months with dogs having ear or genital tumors doing better than dogs with tumors in other locations. Dogs with tumors less than or equal to 3 cm in diameter prior to surgery had a median survival time of 31 months. These are optimistic findings for the Grade III mast cell tumor, even though radiotherapy is an expensive treatment method.
Chemotherapy
When the tumor is no longer localized or is too large for surgery or radiotherapy to control, medication may be helpful to control tumor growth and spread. There are several new medications available and newer ones are constantly being investigated.
Chemotherapy medications that are commonly used currently include: vinblastine (an injection series) usually combined with prednisolone, lomustine (oral or injectable), and toceranib phosphate (oral). Treatment protocols vary in expenses and side effects potential. Discuss with your veterinarian whether referral to a specialist is in the best interest of you and your dog.
Corticosteroids: A Special Mention
Corticosteroids (prednisolone, dexamethasone, etc.) seem to be directly toxic to mast cells and can lead to a brief remission even when used alone. Corticosteroids are inexpensive treatments and definitely worth trying should more powerful chemotherapy drugs be considered too expensive or troublesome.
Tigilanol tiglate: Something New
Tigilanol tiglate (Stelfonta®) is a new treatment released in the summer of 2020 and is best used for dogs where the mast cell tumor cannot be adequately addressed surgically. Tigilanol tiglate is injected directly into the tumor where it interrupts the tumor blood supply, kills the tumor (up to 80% of tumor cells whereas conventional products kill 40-50% of tumor cells), and promotes healing of the area. The injection leads to a great deal of swelling and bruising, followed by an open wound that heals over several weeks. The manufacturer recommends leaving the healing wound uncovered, which may not be acceptable for some pet families.
Treating the Inflammation
The histamine and other inflammatory mediators that are constantly leaked by the mast cell tumor can produce a great deal of inflammation throughout the body. Histamine in particular is a strong stimulus for the production of stomach acid which can lead to stomach ulcers, vomiting, and pain. Antihistamines are frequently used to address the effects of histamine throughout the body. Famotidine is a histamine-blocking antacid commonly used in the palliation of mast cell tumor disease. Other antihistamines such as loratadine and diphenhydramine may be helpful in addressing histamine issues outside of the stomach.
Feline

Courtesy of Dr. Teri Ann Oursler
The mast cell tumor situation is slightly different for cats though most of the same concepts hold true (so if you skipped the canine section to read the feline information it would be best to go back and read it). Mast cell tumors classically affect older cats; in one study the average age was 10 years. There are two forms of feline mast cell tumors: Cutaneous (involving skin) or visceral (involving internal organs, usually intestine or spleen). Tumors are not graded as they are in dogs and staging guidelines are far less defined.
Cutaneous Forms
The skin form of the feline mast cell tumor classically arises around the head, neck, limbs or tail. Lesions may be solitary or multiple, with multiple lesions not necessarily boding poorly (though if there are many mast cell tumors, that would constitute rather a lot of inflammatory biochemicals and more symptoms for the cat). Pathologists classify cutaneous mast cell tumors as either mastocytic or atypical.
Mastocytic mast cell tumors can be further classified as well-differentiated or pleomorphic. Well-differentiated tumors tend to behave benignly and are generally amenable to surgical removal. Most cutaneous mast cell tumors in cats fit into this category. The pleomorphic tumors are more locally aggressive and harder to completely excise. They have more potential to spread in a cancerous fashion.
Atypical cutaneous mast cell tumors erupt in younger adult cats and even kittens. The Siamese breed is predisposed to this unusual tumor type. If possible, atypical tumors should be removed but they have been known to regress spontaneously, which is part of what makes them atypical.
Surgery is the treatment of choice for any cutaneous mast cell tumor.
Visceral Forms
As one might surmise, mast cell tumors located internally are more serious than those in the skin. The most common organs involved are the spleen, liver, and intestine. Vomiting, appetite loss, and weight loss are the most common symptoms. If the spleen is involved, its removal can be very therapeutic; however, results depend on how widespread the disease is. A subset of cats has a median survival time of 12 to 19 months after splenectomy while cats with more disseminated disease have a median survival of 132 days after splenectomy.
No single chemotherapy protocol has emerged as being particularly successful above the others. Unlike the canine situation, it is not all that helpful to stage the disease with buffy coat smears and bone marrow taps as tumor cells in these locations have not altered prognosis, although localizing the disease to the spleen with a splenic aspirate might be particularly useful. The most telling piece of information for prognosis actually comes from the history: appetite. Cats that are eating decently at the time they are first brought to the veterinarian have a median survival of 19 months, while cats that are not eating have a median survival of 8 weeks. Splenectomy is not helpful for cats without splenic involvement.
Not all veterinarians are comfortable treating mast cell cancer. Discuss with your veterinarian whether referral to a cancer specialist would be best for you and your pet.