What is a Disc?
Vertebral discs
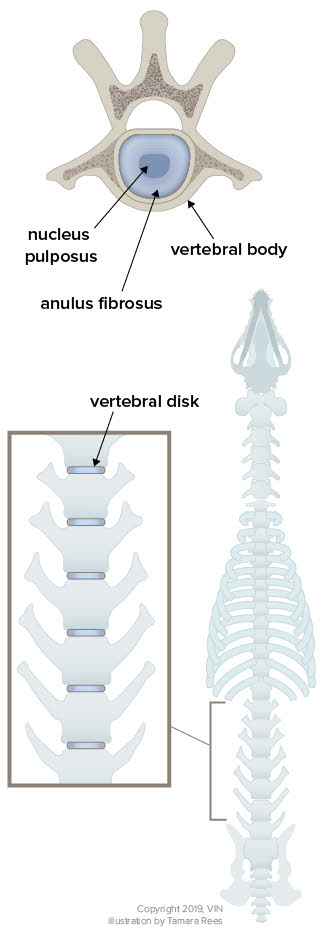
Graphic courtesy of Tamara Rees of VIN
Most people are aware that the backbone is not just one long, tubular bone. The backbone (or spine) is actually made of numerous smaller bones called vertebrae that house and protect the spinal cord. The numerous vertebrae that make up the spine allow for flexibility of the back. The vertebrae are connected by joints called intervertebral discs.
The disc serves as a cushion between the vertebral bodies of the vertebrae. It consists of a fibrous outer shell (called the annulus fibrosus), a jelly-like interior (the nucleus pulposus), and cartilage caps on each side connecting it to the vertebral bones. Ligaments run below and above the discs, with the ligament above the discs being particularly rich in sensitive nerves. These ligaments are called the dorsal (above) and ventral (below) longitudinal ligaments. They run the entire length of the vertebral column.
Canine skeleton disc
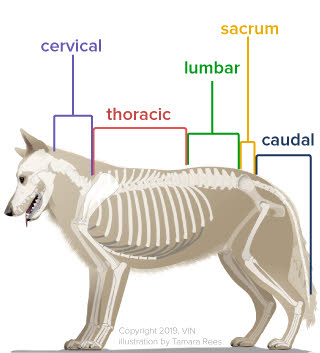
Graphic by Tamara Rees of VIN
There are seven cervical (neck) vertebrae, 13 thoracic (chest) vertebrae, seven lumbar (lower back) vertebrae, three sacral vertebrae (which are fused), and a variable number of tail (caudal) vertebrae.
Type I and Type II Disc Disease
There are two main types of disease that can afflict the intervertebral disc, causing it to press painfully against the spinal cord, nerve roots, and tender dorsal longitudinal ligament: Hansen Type I Disc Disease and Hansen Type II Disc Disease.
In Type I, the nucleus pulposus becomes calcified (mineralized). A wrong jump causes the rock-like disc material to shoot out of the annulus fibrosus. If the disc material shoots upward, it will press painfully on the ligament above and potentially cause compression and bruising of the spinal cord. If it shoots sideways, it will smack into the nerves as they exit the spinal cord. Either way, it is suddenly sharply painful with varying degrees of reduced nerve function.
Twenty-five percent of dachshunds are estimated to have at least one episode of Type I disc disease in their lifetime.
Type II is a much slower degenerative process. The annulus fibrosus collapses and protrudes upward, creating a more chronic problem with pain and spinal cord compression. The disc material impinges on the nerves and spinal cord over months or even years. The German shepherd dog is the poster child for Type II.
The condition where disc material presses against the ligament above and spinal cord is called disc herniation.
The most common sites of disc herniation are T11 - T12 (between the 11th and 12th thoracic vertebrae) and L2 - L3 (between the 2nd and 3rd lumbar vertebrae).
Cervical (neck) disc herniations occur in 15% of disc herniation patients but 80% of these patients are dachshunds, beagles, or poodles.
C2 - C3 (between the 2nd and 3rd cervical vertebrae) is the most common site of disc herniation in the neck.
Symptoms of Disc Herniation
The area of the back or neck just over the disc involved is generally painful (whereas many degenerative spinal processes are not painful). In milder cases, pain at the site of the disc may be the only symptom. As inflammation increases in the spinal cord, neurologic deficits can occur. Disc herniations in the neck tend to have more pain and less dysfunction.
One of the first dysfunctions (or deficits) is the loss of what is called conscious proprioception. Conscious proprioception is the ability to perceive where one’s feet are and orient them properly. The examiner will turn the foot over so that the top of the foot is on the ground and will see if the patient replaces the foot in the proper position. Dogs with poor proprioception will scuff their toes or even occasionally fail to flip their feet while walking and will walk on the tops of their feet. Nerves responsible for conscious proprioception are located on the outside of the spinal cord so when the disc herniates, these nerves feel the pressure first.
After the nerves that affect conscious proprioception go, next are the nerves for voluntary motion (including voluntary control of urination/defecation), followed by the nerves for superficial pain perception, and ultimately the nerves for deep pain perception (usually tested by applying a strong pinch to the toe).
Hansen Type I Disc Herniation
As mentioned, in Hanson Type I disc herniation (also referred to as extrusion), the nucleus pulposus becomes dehydrated and mineralized. It loses its gelatinous cushioning properties and suddenly extrudes, slapping right into the spinal cord and its tender surrounding ligaments. The classic victim is a young dog of a breed that involves a long back and short legs, though any dog can be affected. The damage to the spinal cord can range from mild inflammation to total destruction. Nucleus pulposus is shown in blue.
Hansen Type I Disk Disease
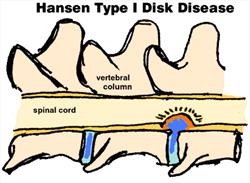
Nucleus pulposus is shown in blue. Normal disk on the left shows nucleus pulposus happily inside the annulus fibrosis. On the right the nucleus pulposus has herniated upward into the dorsal longitudinal ligament and spinal cord, creating swelling and inflammation. (Original graphic by marvistavet.com)
Hansen Type II Disc Herniation
In Type II (also referred to as protrusion), the degeneration is slower and the fibers of the annulus fibrosus become soft. As the disc is compressed by the normal forces between the vertebrae, the annulus fibrosus bulges upwards and puts pressure on the spinal cord more slowly. The classic victim here is an older large breed dog. German Shepherd dogs seem predisposed.
Hansen Type II Disk Disease
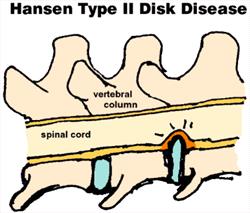
Again the normal disk is on the left (although in this diagram we did not draw in the nucleus pulposus). On the right the disk has been squashed between the adjacent vertebral bodies and the annulus fibrosis is bulging into the dorsal longitudinal ligament and spinal cord. (Original graphic by marvistavet.com)
Diagnostics
With a patient with spinal weakness, the veterinarian must determine whether the problem involves actual compression of the spinal cord. This determination is important because compression can benefit from surgery/anti-inflammatories, while other spinal diseases cannot. Compression in the spinal cord does not have to be from a disc herniation; it could be a vertebral fracture or dislocation, a tumor, or a disc infection. Any of these things could be putting pressure on the spinal cord or nerves and if there is a physical compression, it could – at least in theory - be relieved with surgery.
A non-compressive disease will not benefit from surgery. Such non-compressive diseases include spinal degeneration, spinal infection or inflammation, demyelination injuries, or fibrocartilaginous embolism.
Step One: The Neurologic Examination
By testing different reflexes, the doctor can localize the area of the spinal cord that is affected. This might be the cervical area (neck), the thoracolumbar area (where the chest and abdomen come together), the lumbar (lower back), or the sacral area (where the tail starts). The thoracic (chest) area of the spinal cord is usually spared in disc disease because the ligaments connecting the ribs to the back provide extra protection for the spinal cord.
Step Two: Plain Radiographs
While advanced modes of imaging such as magnetic resonance imaging (MRI) and computed tomography (CT) scanning are not available to most veterinary hospitals, plain radiography usually is. Radiography is also relatively inexpensive compared to other forms of imaging. The first step of imaging typically involves plain radiographs to rule out obvious spinal issues. Broken bones or dislocations are generally obvious. Calcified discs and disc space collapse can often be seen. Radiography of the neck requires general anesthesia or sedation to get proper relaxation of the muscles.
Step Three: Advanced Imaging
If surgery is being considered, then it becomes necessary to identify the exact disc space involved so that the surgeon knows where to cut. Classically, myelography has been the next step, but CT Scanning and even MRI are eclipsing this method. Most hospitals advanced enough to do disc surgery will also be advanced enough for this type of imaging, but we will start with myelography, as it has been the mainstay of diagnosis for decades.
Myelography requires general anesthesia and the injection of iodine-based dye around the spinal cord. The image of the dye can be seen to narrow at the area of spinal cord compression, identifying the area of compression in 85-95% of cases. The patient typically then goes directly to surgery without even waking from anesthesia. If CT is available, a more accurate picture (literally) can be obtained as CT shows cross-sectional images of the area of interest. The calcified disc material can easily be seen smashing into the spinal cord. MRI provides an even better image as all the nuances of different tissue types can be seen. Different classifications of disc disease can be determined.
Treatment
Once it is clear from the plain radiographs and neurologic examination that the patient has disc disease, the decision must be made as to whether or not surgery should be pursued. Spinal surgery is very expensive and requires a long recovery period, but it may be the best choice if the dog is to regain normal function. There are some general rules that are typically applied in making this decision, and they are based on pain and function:
- If the dog can walk, medical (non-surgical) treatment is a reasonable choice but this also depends on how much pain the patient is in, how long the patient has had signs, and what sort of treatments have been unsuccessful in the past.
- The longer the neurologic deficits have been going on, the poorer the results of treatment.
- If the dog cannot walk but has deep pain in at least one limb, there is an 83-93% success rate for recovery with surgery.
- If the dog has been unable to walk and has no deep pain perception in the limbs but has only been down less than 48 hours, success with surgery drops to 50-60%. After 48 hours in this situation, the prognosis is much worse, and it may not be worth considering surgery.
- If the dog cannot walk, medical management may still have success, although surgery is definitely more likely to yield success. Furthermore, return to walking may take months with medical management vs. a few weeks with surgery.
Losing the ability to walk is an emergency. Do not wait to see if it gets better; go to your veterinarian right away!
Medical/Conservative Treatment (No Surgery)
It would be wonderful if there were a magic medication that could completely relieve the pain and inflammation in the spinal cord but, sadly, medications are merely of secondary importance here. While medication can be used to assist in recovery, the centerpiece of therapy is resting the herniated disc through crate or small pen rest. For dogs not already comfortable with a crate, the veterinarian or a qualified behaviorist should be consulted. An owner will be tempted to say that the painful dog will rest himself. In reality, poor results in a dog are almost always traceable to inadequate rest. The dog can be leash walked (or carried) outside to urinate and defecate but then must be walked (or carried) right back in.
Three weeks of cage rest is a minimum course. After this time, the patient can take another two to three weeks to gradually resume regular activity.
Medications typically accompany confinement. Steroids, non-steroidal anti-inflammatories, muscle relaxants, and pain relievers are commonly prescribed. Often the patient is hospitalized for the first week or so of confinement so that cage rest can be accompanied by injectable medications and progress can be monitored. Ice packing applied for 10 to 15 minutes (with a cloth separating the ice pack from the dog) is also helpful in relieving inflammation. During the first 3 to 5 days of an acute episode, icing can be performed as many times daily as possible, ultimately tapering to three times daily for the duration of the confinement or for as long as there is pain.
Physical Therapy (also referred to as Physical Rehabilitation in animals) Exercises During the First 3 to 4 Weeks of Confinement
Exercises should be prescribed by your veterinarian or a rehabilitation veterinarian based on your dog’s progression and healing throughout the rest period. These are the types of exercises that might be prescribed.
- Massage the area gently to improve circulation to the area. This is done as many times a day as possible during the first three to five days, and after that, drop to three times daily.
- Sensory input is important caudal (towards the tail) to the spinal lesion. This entails tickling and pinching the toes. A withdrawal reflex should be elicited. The idea is to make the dog aware of the feet.
- Traction exercise for a lumbar disc issue: (Can be done lying down or standing). Pull the tail at its natural angle for 30 seconds or so. This is done 10 times daily to start and drop down to three times daily by the third week.
Physical Therapy (also referred to as Physical Rehabilitation in animals) Exercises after the Initial 3 to 4 Weeks Confinement Period or with more Chronic Disc Cases
Exercises should be prescribed by your veterinarian or a rehabilitation veterinarian based on your dog’s progression and healing throughout the rest period. These are the types of exercises that might be prescribed.
- Stand the dog up and see how long it takes before they have to sit or lie down. Do not push the dog to exhaustion. For example, if they sit after 30 seconds then the standing exercise should be 20 seconds. Assist standing as needed.
- Stand the dog and gently push them to one side. Do five repetitions three times a day. This is a balance exercise.
- Have the dog sit and then stand. Do five repetitions three times a day. This is a strengthening exercise.
- While the dog is walking, follow along and gently pinch the tip of the tail. This also improves awareness of where the limbs and tail are.
- Walk the dog on lumpy ground. An obstacle course can be made by putting broomsticks or a ladder on the ground, setting up a wastebasket to walk around, etc. The dog should be walked through this three times daily.
- Flexibility exercise involves 60 very small food treats. The dog is standing; assist if needed. Hold the treat up (skyward) so the dog must reach for the treat. This is done 15 times. Hold the treat down at chest level so the dog must reach down for the treat. This is done 15 times. Hold the treat just at the shoulder blade so the dog must reach for it. This is done 15 times on the right and 15 times on the left. Hold the treat back at the level of the hip so the dog must reach around for the treat. This is done 15 times for the right and 15 times for the left.
The dog should at no time be left free to run and jump during the recovery period, even if they seem to be feeling good. Agility, jumping and fetching games or other performance activities are best removed from the dog's lifestyle permanently lest another disc herniate.
Patients who have suddenly lost the ability to walk may be treated conservatively as above but their best chance at regaining the ability to walk is with surgery. Conservative management works best for dogs that are able to walk, have pain perception in their feet, and have both urinary and fecal continence.
These exercises should be prescribed by your veterinarian or a rehabilitation veterinarian based on your dog’s progression and healing. Physical rehabilitation exercises make a huge difference to patient comfort and ability in many situations. Ask your veterinarian about a referral.
Surgery
Spinal surgery is highly invasive, very expensive, and has the potential for great outcomes as well as poor outcomes depending on the damage already sustained by the spinal cord. Patients are generally not candidates for surgery unless they cannot walk, have only been paralyzed for a few days at most, and, of course, have a disease (such as disc herniation) where there is pressure on the spinal cord that can be relieved surgically. There is frequently a great deal of nursing care following surgery, along with physical therapy. Spinal surgery is generally performed on an emergency basis.
The first step will be localizing the area of the compression. A patient may have several areas of disc disease, but the surgeon will need to know which one is the active one. This will require some kind of advanced imaging such as CT scanning, MRI imaging, or myelography. The patient commonly goes directly to surgery after imaging without being awakened from general anesthesia.
Several procedures can be used to decompress the spinal cord and remove the disc material. Several common procedures you may hear about are hemilaminectomy, pediculectomy, dorsal laminectomy, ventral slot, and fenestration.
Hemilaminectomy
This is most commonly performed on disc herniations in the thoracolumbar area. In this surgery, the articular facets (where the two vertebrae connect) are removed, as is the vertebral bone adjacent to the spinal cord. This procedure can safely be performed over up to five adjacent disc spaces.
Pediculectomy
Similar to hemilaminectomy, except only the articular facets are preserved. This is best performed when the disc herniation is slightly off to the side rather than straight upward. This procedure is less invasive and less destabilizing to the vertebrae than hemilaminectomy.
Dorsal Laminectomy
This is probably the most invasive of all the procedures and involves decompressing the spinal cord from the top rather than from the bottom. It can only be done over one disc space and involves removing the dorsal spinous process and lamina, as shown below.
Ventral Slot
This procedure is reserved for neck discs. Here a slot is drilled in the vertebral bodies of the bones on either side of the disc creating a small window over the disc space. Mineralized disc material can be removed and, since the window includes adjacent bone, there is room for the swollen spinal cord to decompress.
Fenestration
This is a preventive procedure often performed on the disc spaces near the herniated space. It involves making a slit over the annulus fibrosus and removing any mineralized nucleus pulposus. In other words, a slit is made in the soft area between vertebrae so that any disc material will herniate away from the spinal cord as it follows the path of least resistance. For some patients, this is the only surgery needed but it is not truly a decompressive surgery. Whether or not fenestration truly reduces the chance of recurrence of signs is a controversial subject.
Recovery after Surgery
The goal of surgery is to restore the pet's quality of life. In most cases, this means the return of the ability to walk. How long it takes the patient to walk again after surgery is highly dependent on how much dysfunction the dog had prior to surgery. Patients with voluntary motor control commonly recovery the ability to walk within two weeks while those with deep pain but no voluntary motor control might require up to 4 weeks. Nursing care for a dog that cannot walk can be intense, including expressing the patient's bladder, keeping the patient bedded, and performing physical therapy exercises. Check with your surgeon regarding the exercises listed above as to which might be recommended for your particular pet.
When the Pet is not Expected to Walk
Taking care of a dog that is down in the back is a big project and definitely not something that every dog owner is able to commit to. Still, it can be done, and for the right dog and the right person, it is a highly rewarding experience. A great deal of progress can often be made using physical therapy exercises as described in the medical management section, plus there are a number of resources and products available to assist in caring for an immobile pet.
Physical Rehabilitation
Physical rehabilitation exercises make a huge difference to patient comfort and ability in many situations. Discuss with your veterinarian whether referral to a specialist would be best for you and your pet.