Your 8-year-old yellow Lab Tinker Bell just came in from the backyard and you notice she’s limping on one of her back legs. You check the medicine cabinet in your bathroom to see what medications you have that may help her feel better. You see bottles of aspirin, ibuprofen, naproxen, and acetaminophen—all pain relievers for people. You also have a few tablets of carprofen left over from when your other dog had knee surgery. Before reaching for any of the bottles, STOP and call your veterinarian. A pain reliever meant for you or even for your other dog may not be right for Tinker Bell and may even hurt her.
Nonsteroidal Anti-Inflammatory Drugs
Veterinary Partner Note:
Never give human medications to pets without speaking with your veterinarian. Giving some over-the-counter human medications to pets can cause severe illness and even death.
With the notable exception of acetaminophen, all the medications listed in the introduction are nonsteroidal anti-inflammatory drugs, commonly called NSAIDs. These drugs are widely used in both people and animals for their pain-relieving, anti-inflammatory properties. Veterinarians often prescribe NSAIDS for dogs with osteoarthritis, a condition where cartilage - the protective material that cushions a joint between two bones - breaks down over time, causing the bones to rub against each other. This rubbing can permanently damage the joint and cause pain, inflammation, and lameness. Veterinarians also often use NSAIDs to manage pain after surgery in both dogs and cats.
The Science — How NSAIDs Work
Nonsteroidal anti-inflammatory drugs reduce pain and inflammation by affecting substances that the body releases after cells are damaged. When a cell is damaged, an enzyme called cyclooxygenase (COX) is activated. Essential to all body functions, enzymes are proteins made by the body and are very specific—each enzyme stimulates a specific reaction that causes a specific result. In the case of the enzyme COX, it stimulates cells to produce several substances, including prostaglandins, after the cells are damaged. COX is present in most body tissues, including the digestive tract (stomach and intestines) and kidneys.
Like COX, prostaglandins are present throughout the body. These substances contribute to pain and inflammation, but they have several positive functions too, including:
- Protecting the lining of the stomach and intestines;
- Helping maintain blood flow to the kidneys; and
- Supporting platelet function (platelets are found in the blood of all mammals and help with blood clotting).
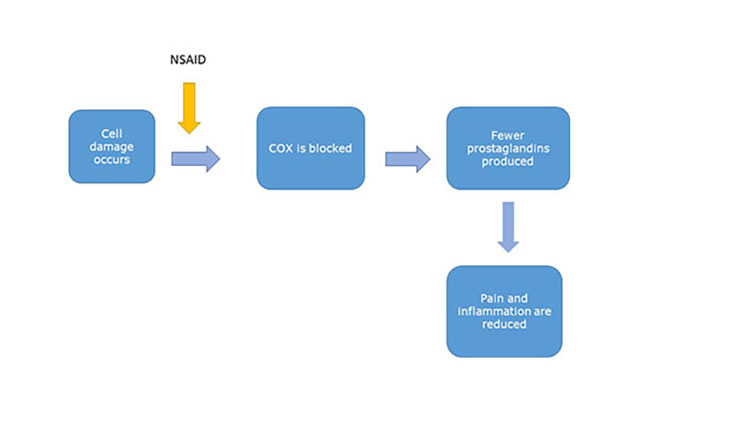
Many NSAIDs work by blocking COX, so fewer prostaglandins are produced:
Other NSAIDs work by blocking some activity of certain prostaglandins:
Mainly by either blocking COX or blocking some activity of certain prostaglandins, NSAIDs reduce ongoing pain and inflammation in animals.
Side Effects
Because NSAIDs interfere with prostaglandins, including their positive functions, the drugs can cause side effects. Some of the most common side effects of NSAIDs in dogs and cats reported to FDA’s Center for Veterinary Medicine are:
- Vomiting
- Decreased to no appetite
- Decreased activity level, and
- Diarrhea.
Other, more serious side effects in dogs and cats include ulcers in the stomach and intestines, perforations (holes) in the stomach and intestines, kidney failure, liver failure, and even death in some cases.
The side effects of NSAIDs are mainly seen in the digestive tract, kidneys, and liver.
The Digestive Tract (Stomach and Intestines)
Nonsteroidal anti-inflammatory drugs can cause side effects in the digestive tract both directly and indirectly. The direct effects are related to the drugs’ physical properties. Many NSAIDs become trapped in the stomach and are slightly acidic, so they directly irritate the stomach lining.
The indirect effects are due to NSAIDs either preventing the body from making prostaglandins or blocking the protective activity of these substances. Remember, prostaglandins also protect the lining of the stomach and intestines. When fewer prostaglandins are produced or some of their activity is blocked, the entire digestive tract may be more prone to damage. This can lead to ulcers and perforations (holes) in the stomach and intestines.
Giving an animal two NSAIDs at the same time, or an NSAID with a steroid such as prednisone, increases the risk of side effects in the digestive tract and should be avoided.
Side Effects in the Kidneys
During periods of decreased blood flow to the kidneys—such as when an animal is dehydrated, under anesthesia, or has kidney disease—prostaglandins cause the arteries going to the kidneys to open. This helps keep blood flowing to these vital organs.
Because NSAIDS prevent the production of prostaglandins or block some prostaglandin activity, these drugs can reduce blood flow to the kidneys, possibly causing kidney damage and leading to sudden-onset kidney failure.
NSAIDs should be used cautiously in animals that may already have kidney disease or other conditions that cause reduced blood flow to the kidneys, like dehydration and shock. If an NSAID is used around the time of surgery, intravenous (IV) fluids are generally recommended before, during, and after anesthesia to maintain blood flow to the kidneys, hopefully reducing potential kidney complications.
Side Effects in the Liver
The side effects of NSAIDs on the liver can be divided into two categories: (1) dose-dependent; and (2) dose-independent.
As the name implies, dose-dependent side effects are related to the dose—the higher the dose of the NSAID, the worse the side effects and the liver damage. This type of liver damage is typically caused by a massive NSAID overdose, such as a dog eating an entire bottle of his owner’s ibuprofen. (The ASPCA Animal Poison Control Center receives hundreds of calls each year involving dogs and cats that accidentally eat nonsteroidal anti-inflammatory drugs.)
Remember to keep all medications—for both people and pets—in a secure location out of reach of children, dogs, cats, and other animals to prevent accidental ingestion or overdose.
Dose-independent side effects can occur at any dose of an NSAID, even the correct one, and is an unpredictable reaction where the patient’s liver has an abnormal sensitivity to the medication. Most liver damage that is associated with an NSAID occurs within the first three weeks of starting the medication.
NSAIDs should be used cautiously in animals that may already have liver disease.
FDA-Approved NSAIDs for Pets
The table below lists the currently marketed FDA-approved NSAIDs for dogs and cats. All of them are available by a veterinarian’s prescription only. No over-the-counter NSAIDs for dogs and cats are FDA-approved. Any NSAID marketed for dogs or cats online or in a pet store without the need for a prescription from a veterinarian is an unapproved animal drug, meaning FDA has not reviewed information about the drug. An unapproved animal drug may not meet the agency’s strict standards for safety and effectiveness and may not be properly manufactured or properly labeled.
| Species |
| Carprofen |
Marketed under multiple trade names |
Dogs only |
| Deracoxib |
DERAMAXX, DOXIDYL* |
Dogs only |
| Firocoxib |
PREVICOX |
Dogs only |
| Grapiprant |
GALLIPRANT |
Dogs only |
| Meloxicam |
Marketed under multiple trade names |
Dogs (injectable, oral) and cats (injectable only) |
| Robenacoxib |
ONSIOR (for a maximum of 3 days) |
Dogs and cats |
*Indicates an FDA-approved generic animal drug.
NSAIDS for Dogs
Several NSAIDs are FDA-approved for dogs to control pain and inflammation associated with osteoarthritis; and to control pain and inflammation after soft tissue and orthopedic surgery. [Orthopedic pertains to bones and muscles; soft tissue is everything else. Repairing a dog’s torn ACL (anterior cruciate ligament) in her knee is an orthopedic surgery; removing a ball from a dog’s stomach is a soft tissue surgery.]
Most of the NSAIDs for dogs listed in the above table are approved for both uses (for osteoarthritis and after surgery) with two exceptions: (1) robenacoxib (sold under the brand name ONSIOR) is only approved to control pain and inflammation after soft tissue surgery and should be given for a maximum of 3 days; and (2) grapiprant (sold under the brand name GALLIPRANT) is only approved to control pain and inflammation associated with osteoarthritis.
All NSAIDs for dogs are given either by mouth (oral) or by injection.
Monitor Dogs on Long-Term NSAIDs
Because osteoarthritis is a long-term (chronic) condition that doesn’t go away, a dog may be on an NSAID for a long time. The lowest dose that provides adequate pain control should be used. Owners should always consult with their veterinarian before adjusting the dose, especially before increasing it.
For a dog taking an NSAID long-term for osteoarthritis, it’s good to check his or her liver and kidney function by doing blood tests before starting the medication and then repeating the blood tests on a regular basis.
NSAIDs for Cats
Only two NSAIDs are FDA-approved for cats: meloxicam (sold under several brand and generic names) and robenacoxib (sold under the brand name ONSIOR).
Meloxicam is approved for cats as a one-time-only injection to control pain and inflammation after spaying, neutering, and orthopedic surgery. The injection is given under the cat’s skin before surgery.
Robenacoxib is also approved for cats to control pain and inflammation after spaying, neutering, and orthopedic surgery. The medication should be used once daily for no more than three days and is available as either a tablet given by mouth or an injection given under the cat’s skin.
No Long-Term NSAIDs for Cats
Currently, no NSAIDs are approved for long-term use in cats. Cats are especially sensitive to the side effects of NSAIDs. More than one dose (repeated doses) of meloxicam in cats can cause kidney failure or death, and more than three doses of robenacoxib have not been shown to be safe in cats.
Benefits of Using FDA-Approved NSAIDs for Dogs and Cats
A main benefit of an FDA-approved nonsteroidal anti-inflammatory drug for dogs or cats is that it has been shown to be safe and effective in that species when used according to the label. NSAIDs for people or unapproved NSAIDs for animals don’t have the same assurances of safety and effectiveness in pets and could be harmful.
A second main benefit is that the label for an FDA-approved NSAID for dogs or cats is written specifically for that species. The label includes all the information veterinarians need to use the drug safely and effectively in that species.
A Balancing Act—Benefits versus Risks
FDA-approved nonsteroidal anti-inflammatory drugs offer pain relief for many dogs with osteoarthritis. These drugs also help veterinarians effectively manage pain after surgery in both dogs and cats. Yet, there are risks.
NSAIDs account for a large number of side effects in dogs and cats that are reported to FDA’s Center for Veterinary Medicine. While any dog or cat can have a side effect to an NSAID, the two most common groups of pets that receive NSAIDs may have additional risk factors that need to be considered:
- Dogs with osteoarthritis. These dogs are usually older and may have another disease in addition to osteoarthritis, such as kidney or liver disease.
- Surgery patients. These dogs and cats were recently under anesthesia which reduces blood flow to the kidneys.
Risk Reduction
FDA’s Center for Veterinary Medicine tries to reduce the risks of side effects associated with NSAIDs by working with drug companies to write clear, thorough drug labels for veterinarians and Client Information Sheets for owners.
Every oral NSAID approved for dogs and cats has an accompanying Client Information Sheet for veterinarians to give owners the first time the prescription is filled and each time it's refilled. You should ask for this sheet if you aren’t given one. It summarizes important safety information about the drug and serves as an easy reference for you at home.
The label of every approved NSAID for pets has a section called “Information for Dog Owners” or “Information for Cat Owners.” Before using the drug in your pet, your veterinarian should discuss the information in this section with you.
Over-the-Counter NSAIDs for People- Are They Safe for Pets?
The table below lists some common over-the-counter NSAIDs for people.
| Aspirin |
ASCRIPTIN, BAYER, BUFFERIN, ECOTRIN |
| Ibuprofen |
ADVIL, MOTRIN |
| Naproxen sodium |
ALEVE, MIDOL EXTENDED RELIEF, NAPROSYN |
Dogs are Not Small People.
Tinker Bell’s owner isn’t alone. When owners see their dog or cat limping or showing other signs of pain, they often think about giving their pet an over-the-counter pain reliever for people. But even if data show an NSAID is safe and effective in people, the drug may not be safe and effective in dogs because the drug may:
- Last longer;
- Be absorbed faster by the stomach and intestines; and
- Reach higher blood levels.
Cats are Not Small People or Small Dogs.
You have to be even more careful with cats. Compared to other species, cats may have a reduced ability to break down NSAIDs.
Only People are People
These differences between people and pets may lead to worse side effects in pets if they're given NSAIDs for people.
Acetaminophen (TYLENOL)—A Special Case
Acetaminophen (most commonly known as its brand name TYLENOL) is not a nonsteroidal anti-inflammatory drug. It's an over-the-counter pain reliever for people, but doesn’t have much anti-inflammatory activity. Scientists don’t fully understand how acetaminophen works to relieve painExternal Link Disclaimer.
Acetaminophen can cause two main forms of side effects in dogs and catsExternal Link Disclaimer:
- Dose-dependent liver damage—meaning the higher the dose, the worse the liver damage—that may lead to liver failure; and
- Red blood cell damage that causes these cells to lose their ability to carry oxygen.
Dogs and cats can suffer both forms of side effects from acetaminophen, but cats are more prone to red blood cell damage while dogs are more likely to get liver damage.
Veterinarians will sometimes use acetaminophen to relieve pain in dogs but never in cats. Acetaminophen is fatal to cats.
Cats should never be given acetaminophen because they lack certain enzymes that the liver needs to safely break down the drug.
What Should you Do?
- Before giving any NSAID to your dog or cat, talk with your veterinarian. Tell him or her if your pet:
- Has a history of digestive problems, such as stomach or intestinal ulcers, or has had surgery on the stomach or intestines. Even if your pet hasn’t had any digestive problems in the past, that doesn’t mean he or she has a healthy digestive tract. Dogs and cats can have stomach and intestinal ulcers or other digestive problems without showing signs.
- Is on any other prescription or over-the-counter medication. Two different NSAIDs, or an NSAID and a steroid, should not be given at the same time.
- While your pet is taking an NSAID and for a little while after he or she stops taking it, monitor him or her for side effects, such as
- Vomiting,
- Diarrhea,
- Bloody or black stool,
- Decreased appetite,
- Decreased activity level, and
- Yellowing of the whites of the eyes or the gums.
These signs can occur even in a previously healthy pet. If you notice any side effects, stop giving the medication and call your veterinarian.
- If your pet has a side effect to an NSAID, FDA’s Center for Veterinary Medicine encourages you to work with your veterinarian to report the problem.
- Before starting your dog on an NSAID long-term for osteoarthritis, ask your veterinarian about performing baseline blood tests. Talk to your veterinarian about how often to recheck your dog’s blood tests.
- No NSAID is currently FDA-approved for long-term use in cats.
- Keep all medications—for both people and pets—in a secure location out of reach of children, dogs, cats, and other animals to prevent accidental ingestion or overdose.
Luckily, Tinker Bell’s owner closed the medicine cabinet and called her veterinarian first. Tinker Bell got on the right medication for her and is bouncing around the backyard once more. Be like Tinker Bell’s owner and be safe—don’t give any medication to your pet until you talk to your veterinarian.