What is Helicobacter?
Helicobacter is a genus of spiral bacteria that, amazingly, is able to survive the severe acidity of the stomach. The existence of such bacteria has been known of since 1889, but it wasn't until nearly 100 years later that their significance was realized.
Until the 1980s, stomach ulcers were treated with an assortment of antacids with the idea that excess acid had caused the ulcer. It turned out that most stomach ulcers of humans weren't from excess stomach acid but were from Helicobacter infection instead. Treatment is aimed at both reducing stomach acid and killing Helicobacter.
Currently, this ulcerative infection is treated with medications that reduce stomach acid secretion combined with antibiotics specifically directed against Helicobacter.
The relationship between Helicobacter and stomach ulceration is not simple. Stress plays a part as does concurrent disease. Most dogs and cats harbor Helicobacter in their stomachs and never get sick as a result but in the right circumstances, a Helicobacter infection can complicate other intestinal disease.
How Does Helicobacter Cause Damage?
Very few organisms can withstand the extreme acidity of the stomach. The tissue of the stomach is protected by a layer of mucus into which bicarbonate is secreted as an acid neutralizer. The integrity of this mucus lining keeps us from being burned by our own stomach acid.
Helicobacter survives by using enzymes to create its own layer of protective bicarbonate. This little safety suit allows the bacteria to actually burrow into the stomach without regard for the extreme acid surrounding it. The presence of Helicobacter generates inflammation in the stomach tissue.
Many patients are colonized by Helicobacter and do not develop symptoms; however, if Helicobacter penetrates deeply enough, it will bind to the mucus-secreting cells of the stomach and disrupt their ability to produce normal mucus. Ultimately, the stomach's mucus lining is disrupted, acid gains access to the stomach tissue, and burning results.
Ulcers are thus formed. Making matters worse, Helicobacter organisms are able to stimulate extra acid secretion by the stomach tissue. More burning and more ulcers result, and soon the patient is experiencing pain, nausea, and/or vomiting. It is unclear what constitutes a few Helicobacter bacteria sharing the stomach with its host peacefully and numerous Helicobacter organisms disrupting the stomach lining integrity and causing disease. It is possible that without additional stomach disease (such as inflammatory bowel disease) or other factors (stress, anxiety), Helicobacter causes no trouble. there are many strains and types of Helicobacter, and not all of them cause harm. Helicobacter organisms are often found in small numbers in normal stomachs.
Some Helicobacter species are also capable of producing toxins, but the role of such toxins in this disease process is not clear.
Helicobacter seems to be one reason why an animal that has been stable with inflammatory bowel disease or some other stomach disease might suddenly get much worse.
It is unclear what constitutes a few Helicobacter bacteria sharing the stomach with its host peacefully versus numerous Helicobacter organisms disrupting the stomach lining integrity and causing disease. It is possible that without additional stomach disease (such as inflammatory bowel disease) or other factors (stress, anxiety), Helicobacter causes no trouble. Complicating the picture is the fact that there are many strains and types of Helicobacter and not all of them cause harm. Helicobacter organisms are often found in small numbers in normal stomachs.
Does Helicobacter Infection Cause Cancer?
In humans, it appears that Helicobacter infection may indeed cause cancer. In people, Helicobacter infection represents a 400% risk increase for the development of stomach cancer. Pets, however, get infected with different Helicobacter species, and the same association with cancer in these species has not been made.
Does My Pet Have Helicobacter Overgrowth?
There are many excellent ways to determine if a pet's chronic gastrointestinal problem is complicated by Helicobacter infection.
Biopsy
While it is possible to miss Helicobacter if only certain areas of the stomach are colonized, a biopsy is by far the most accurate test. This method not only detects the infection but also assesses the degree of inflammation and checks for cancer.
Helicobacter On Cytology
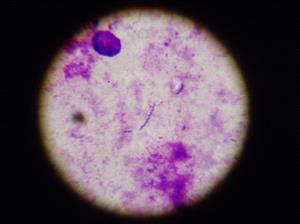
Impression smears from gastric endoscopic biopsy. Photo Courtesy Dr. Adam Honeckman.
The Rapid Urease Test
Some gastroenterologists will keep a special broth handy during the biopsy procedure. A spare tissue sample can be dropped in the broth and incubated for an hour. The presence of urease, the enzyme that creates Helicobacter's protective bicarbonate layer, induces a color change in the solution. In this way, Helicobacter can be detected in an hour rather than after the several-day periods it takes to obtain biopsy results.
PCR Testing
This especially sensitive DNA testing can be used but is only available in a few centers.
Blood Tests
Antibodies against Helicobacter can be detected, but their levels take months to decline even after the Helicobacter organism is long gone, limiting the usefulness of such testing.
Breath Testing
A radioisotope-labeled meal is fed, and the patient's breath is tested for Helicobacter metabolites. This form of testing is easy to use for monitoring the eradication of Helicobacter, plus it is non-invasive. In humans, Helicobacter eradication is usually confirmed four to eight weeks after treatment has been completed. With the breath test, a second biopsy or endoscopy is not needed. Unfortunately, this type of testing is not readily available for pets.
What is the Treatment?
Treatment protocols generally consist of two or three antibiotics and a medication to reduce stomach acid production. Numerous medication combinations have been used. Treatment typically involves two to three weeks of medication use.
Here is a list of medications typically used in the treatment of Helicobacter:
Can My Pet Infect Me?
Currently, this is not known. At least one known Helicobacter species is capable of infecting both humans and cats. Cat ownership does not seem to represent an increased risk for Helicobacter infection in humans. Transmission of the disease is felt to be through contact with vomit or fecal matter. When cleaning up after your pet, wear gloves if possible, and certainly wash your hands thoroughly afterward.